Cycling Gave Me Urinary Problems and Erectile Dysfunction
A self-limited episode of urinary hesitancy, urinary retention, dysuria, erectile dysfunction, and raised PSA level followed a moderate level of road cycling.
Although ulcerative colitis is my most serious medical problem, and irritable bowel syndrome is my most vexing on a day-to-day basis, the most prominent health issue I have had to deal with since the start of the current local COVID-19 lockdown (aka Movement Control Order, MCO) period related to my urinary and erectile function – this indeed came from left field!
My symptoms had resolved completely by the first week of April, though the lingering worry was a mildly raised prostate-specific antigen (PSA) level on April 16, 2020. I had a repeat PSA test yesterday, i.e. June 3, 2020 – I’m overjoyed the level is back within the normal age-adjusted range.
With my urinary tract, membrum virile, and prostate functioning normally again, I thought I’d write up the episode to record my analysis of what might have happened in and around my perineum from a moderate amount of cycling that led to my woes in the past few months.
My Urinary Symptoms
I’ll first describe my urinary symptoms.
Urinary hesitancy and urinary retention
In retrospect, the first symptom was a weaker-than-normal urine stream, beginning around late February or early March 2020. Over about three weeks, this became increasingly more noticeable, accompanied by other symptoms of urinary hesitancy, e.g., delay in initiating a urine stream, difficulty maintaining a stream, and weak stream. Unsurprisingly, the time needed to empty my bladder was also getting longer and longer.
By March 20, 2020, the urinary flow had weakened to short spurts and dribbling, with incomplete emptying of my bladder. And because I couldn’t empty my bladder, I had to pee at brief intervals, i.e., I had urinary frequency.
Also, my symptoms were noticeably worse overnight. For about five days, i.e., from March 20–25, 2020, I would invariably experience extreme urinary hesitancy, taking 5–10 minutes to start a stream (with some straining), producing a weak stream (so not much of a urine flow), and inability to maintain a stream even with a lot of strain. From March 21, 2020, I used a plastic container to collect the urine I passed and measured its volume. On each trip during the day, I’d consider myself lucky if I passed more than 100 mL or 3.38 fl oz. However, the amount was even less at night, and the time to pass that small amount felt like forever. It felt like I was forcing my urine through a tiny pinhole. I got little sleep on those few nights because of the frequent trips to the bathroom and constant uncomfortable feeling of fullness in my bladder (and anxiety over the possibility of the nanoscopic hole in my urinary tract would spontaneously close).
This turn of events was unexpected. I had presumed my mild urinary hesitancy (during the initial phase of this entire episode) was part of aging, but having such difficulties in urination for a guy in his mid-forties with no history of urological problems was abnormal.
There was a point in time, perhaps on the evening of March 21, 2020, that I considered the possibility of acute complete urinary retention, especially overnight. The prospect of this emergency led me to (A) search my storeroom for equipment to perform a suprapubic puncture, and because I couldn’t find the right equipment, (B) on March 22, 2020, to walk to the nearby pharmacy (which did not have the equipment either). So I made do with whatever gear I already had on hand in case of an emergency. Fortunately, my symptoms never called for the need for a suprapubic puncture.
Pain on urination
On those days and nights when the urinary hesitancy was severe, I also experienced pain in my perineum and glans penis during and after urination. The post-void pain was more severe (Numeric Rating Scale (NRS): 7) than that while peeing. The pain was shooting and tingling in nature and would typically last anywhere between 30 and 60 minutes post-void.
Besides the pain above, I felt a sense of constant fullness in my perineum that was not relieved by urination. It was “always there,” no matter how much urine I passed. I suspect this sensation was from my prostate, but I have no way of confirming this.
Erectile Dysfunction
From about when my urinary symptoms started, i.e., late February or early March 2020, I also had erectile dysfunction. This problem continued until my urinary symptoms resolved in the first week of April 2020.
Other Relevant Information
I didn’t have a fever. Most of the time, I could feel my bladder only partially emptied post-void, but I wouldn’t regard this sensation as pain. The urine appeared normal – the color looked no different from what it had been in the past several months (clear light yellow); there was no cloudiness and no change in odor. I did not see any urethral discharge.
There wasn’t any genital numbness. I had no change in my bowel habit, and sensation in my rectum, anus and perianal region was normal. I did not have any urinary or fecal incontinence.
I’ve had many medical problems, but they never included urinary tract infections or kidney stones. I have had no sexually transmitted disease (STD) and had no reason to have one. Further, I don’t have diabetes mellitus or other endocrine or metabolic disorders.
A possible contributing factor to my urinary symptoms was the anticholinergic drugs I was taking for my irritable bowel syndrome – Liblan (chlordiazepoxide + clidinium bromide) and amitriptyline. These two drugs were unlikely to have caused my symptoms – I had taken them for over two years – but they could have worsened my symptoms. I stopped taking both drugs on March 22, 2020. There was no improvement immediately after I stopped taking them, but my urinary symptoms did not worsen.
Cycling: The Elephant in the Room
As I thought about the cause of my symptoms, I couldn’t help wondering about the part cycling played. It was uncomfortable considering whether my favorite pastime was the root of my present health issues.
Video showing the contact between the perineum and bicycle saddle.
Cycling log
I hadn’t done much cycling before my urinary problems began. I was out of town for work in the first week of March 2020, so I didn’t cycle that week.
The following is information on my cycling in March 2020, as recorded in Strava.
| Date and Time | Distance (km) | Average Speed (km/h) | Maximum Speed (km/h) |
|---|---|---|---|
| March 9, 2020 (MON) @23:58hrs | 31.96 | 28.5 | 40.7 |
| March 12, 2020 (THU) @17:22hrs | 4.10 | 22.0 | 45.7 |
| March 12, 2020 (THU) @18:23hrs | 7.78 | 24.6 | 42.5 |
| March 13, 2020 (FRI) @00:05hrs | 21.16 | 25.5 | 43.9 |
| March 13, 2020 (FRI) @15:24hrs | 4.89 | 26.8 | 41.4 |
| March 13, 2020 (FRI) @15:47hrs | 5.35 | 27.4 | 46.1 |
| March 17, 2020 (TUE) @00:12hrs | 31.92 | 29.5 | 45.0 |
| Total distance in March 2020 | 107.16 |
Below are the details that explain the data in the table.
On March 9, 2020, I went on a solo night ride (31.96 km).
On March 12, 2020, I rode my Giant TCR Advanced bike to the Giant Bicycles store, also my local bike shop (LBS), to upgrade its wheels. I chose a set of Shimano Dura-Ace R9100 C40 clinchers.

In the early hours of the next day (5 minutes past midnight, to be exact), I took my bike out for a ride. The plastic spoke protector on the rear wheel kept coming off on that ride, giving an irritating rattling sound. It fell off after a few minutes whenever I put it back on. The spoke protector had stayed on when I rode home from the bike shop the previous day. Because of the trouble with the loose spoke protector that night, I called it quits mid-ride.
The spoke protector didn’t stay on because Giant designed it to work with its road wheels, which have round spokes. The Shimano wheels have bladed spokes.
So I took the bike to the shop the same day (March 13, 2020) to remove the spoke protector.
On March 17, 2020 – one day before the local lockdown came into force – I went out for a ride (and broke some personal records).
I did not sit on the saddle between March 17, 2020, and May 20, 2020, because of the lockdown (which did not permit cycling outdoors) and for fear of aggravating my symptoms. From May 20, 2020, my symptoms became noticeably worse.
Unpadded cycling shorts
On both trips to my local bike shop on March 12 and 13, 2020, I wore a pair of God & Famous commuter shorts, which are unpadded. I prefer to wear these when I’m not doing “serious” cycling because they blend in more easily than my cycling shorts. Wearing my G&F shorts was probably a mistake – though my favorite, they don’t offer any meaningful shock-dampening protection to my perineum.
Saddle in a neutral position
In the first week of March, I also fiddled with the tilt angle of my saddle, and I believe it ended up in a neutral position (i.e., zero tilt), as opposed to a slight downward, forward tilt it had since February 21, 2020. A neutral position was probably too high (compared to a slightly lowered saddle nose) for my speed-oriented cycling style and created too much pressure on my perineum when I was in the drops (where I spend at least 80% of my time). After one ride, I tilted the nose of the saddle downwards by 2°, i.e., back to where it was initially. I cannot be sure, but I suspect the 2° downward, forward tilt has helped relieve pressure on my perineum, especially when I am in an aggressive position. I’m tempted to lower the saddle nose by another couple of millimeters.
Lower bicycle stem height
My records show I dropped my bicycle stem height by 17 millimeters on February 20, 2020. (I wouldn’t have looked this up if I wasn’t writing this blog post.) The drop in stem height was probably a contributing factor to the trouble in my perineum. I might have had a neutral saddle position previously, but with the reduction in stem height, it would have been prudent to have the front of the saddle tilted downward a little to lessen perineal pressure.
Selle SMP Dynamic Bicycle Saddle
Since we’re on the topic of my bike saddle, I think I should mention some details about it. I found the saddle that came stock with my bike quite uncomfortable – my ischial tuberosities would be sore during each ride and continue to ache for a few days afterward.
My solution was to change the saddle to a Selle SMP Dynamic on February 21, 2020. This saddle is a lot comfier than the Giant stock saddle – no more pain during or after the ride.
The middle cutout of this saddle is relatively wide and long, and its heavily contoured shape acts like a car bucket seat, limiting fore and aft movement on the saddle. Therefore, it seems unlikely there would be pressure on my perineum once I’m on/in the saddle.


However, I sometimes noticed the nose of the saddle pushing against my perineum, especially when dismounting. I put this down to poor technique, which I’ve corrected since March 13, 2020. I don’t know the extent of injury the occasional contact with my perineum caused to the underlying structures.
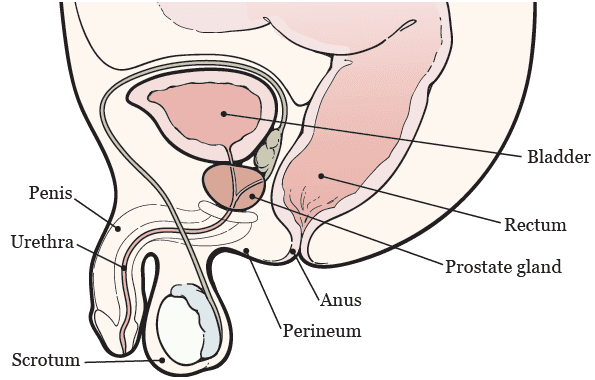
Anatomy
In writing up this post, I had to review some anatomy of the male pelvic viscera and their relationship with the perineum, where the saddle comes into contact. The diagram below shows that there is only a tiny space, the ischioanal fossa, between the perineum and the urethra and prostate. The ischioanal fossae (there are two; one on the left and one on the right) are essentially fat pads. Based on the subcutaneous fat in my body, I cannot imagine I have much in these two regions.
The following video helped me better understand the anatomy of the branches of the internal pudendal artery and the pudendal nerve, structures vulnerable to injury with excessive or prolonged pressure on the perineum.
Annotated anatomy video: branches of the internal pudendal artery and pudendal nerve. Video: Dr James Pickering, Faculty of Biological Sciences, University of Leeds. Source: YouTube
Differential Diagnosis
Before seeing a urologist on March 26, 2020, I naturally had a list of possible diagnoses to explain my symptoms (listed below, not in order of probability):
1. Urinary tract infection. At first glance, it might have seemed I had a urinary tract infection (UTI). However, factors against a UTI included being male, no known obstruction, no instrumentation of the urinary tract (ever), and no urologic surgery.
2. Acute Prostatitis. If I had acute prostatitis, I would have expected more symptoms to suggest infection, and I could have experienced more severe and more constant pain in/from my prostate and a fever.
3. Urethritis. Inflammation of the urethra was another possibility. Again, the lack of signs of infection (as opposed to symptoms) pointed against this diagnosis.
4. Enlarged prostate. An enlarged prostate could have explained my symptoms. However, the rapid development of urinary symptoms made prostatic enlargement less likely.
5. Urethral stricture. It certainly felt like I had a urethral stricture. But I did not have any known risk factors, e.g., trauma or surgery, catheterization, radiation, or enlarged prostate.
7. Kidney stone lodged in the urethra. A kidney stone might have lodged in my urethra, hence causing the symptoms I was experiencing. I had no known risk factors for kidney stones.
The major problem with all the diagnoses above was that they did not explain the erectile dysfunction accompanying the urinary symptoms.
8. Bicycle seat neuropathy. Also called cyclist syndrome, pudendal neuropathy, pudendal neuralgia, pudendal nerve entrapment syndrome, and Alcock canal syndrome, bicycle seat neuropathy is relatively common among cyclists. Though well documented in the medical literature, this condition was new to me; I first heard of it on a Global Cycling Network (GCN) YouTube video on preventing saddle-related numbness and discomfort. In that video, GCN’s Daniel Lloyd offers valuable tips on alleviating pressure on the perineum while cycling. A pressure effect on the perineum from the saddle and subsequent injury – either ischemic or compressive – to the pudendal nerve or one or more of its branches causes bicycle seat neuropathy, which has different presentations. This condition would account for all my symptoms: the urinary dysfunction, the neuropathic pain in the perineum and glans penis, and erectile dysfunction.
What I Did Before Seeking an Expert Opinion
By the evening of March 25, 2020, I had enough. DIY medicine can only take you so far. It was time to see a specialist.
My symptoms were not getting any better, despite being off the two anticholinergic drugs for a few days and drinking lots of water (in case I had a urinary tract infection, but in hindsight, doing this exacerbated my urinary symptoms). I had disrupted sleep over several nights, and I felt moody during the day.
Double Voiding: My Version
I discovered that peeing twice every time I felt the need to go to the loo helped me empty my bladder better than trying to pass everything in one go. A few days after I started doing this, I learned this technique is called double voiding. My version of double voiding took anything between 10 and 20 minutes between efforts to pee, this interval being longer than the conventional idea of double voiding. Taking my mind off the incompletely emptied bladder, e.g., by watching a YouTube video or resuming writing a report, during breaks was extremely helpful. The interval also allowed me to recover from the straining I did in the first effort. I would continue to double void till the first week of April, when my symptoms resolved, and the amount of urine passed per effort was at least 350 mL.
Urology Outpatient Appointment on March 26, 2020
On the morning of March 26, 2020, I saw a consultant urologist (Dr TCL) in his clinic.
As expected, he ordered a mid-stream urine (MSU) test. The results came back within a few hours, probably because there were few patients in the hospital because of the COVID-19 lockdown. My urine was normal, with no evidence of infection or blood in the urine (hematuria).
A transabdominal ultrasound scan showed a normal-sized prostate gland.
My urologist thought the problem was “multi-factorial,” which included some injury to my prostate because of the cycling. He recommended I stop cycling altogether, which would not be a problem since the authorities had banned road cycling during the lockdown period. But there was little chance I would quit cycling for good.
Dr TCL ordered a prostate-specific antigen (PSA) test – I would have this done together with blood tests scheduled on the same day as the outpatient appointment with my gastroenterologist about three weeks later. He also prescribed terazosin (Hytrin), an α-blocker, 1 mg once a day at bedtime.
Progress
Over the next few days, all my symptoms seemed to improve gradually. I’m uncertain how much the small dose terazosin helped – I wasn’t suffering any adverse effects, so I didn’t mind taking it. I continue to do so on my doctor’s advice.
My symptoms disappeared entirely by the first week of April 2020.
On the day I was due to see my gastroenterologist (April 16, 2020), I had a few investigations done, including the PSA test. The PSA level was near-normal at 4.01 ng/mL (reference range 0–4). I wasn’t too concerned about that result, but according to my urologist, this level should have been lower than what the laboratory reference range suggested. He told me the upper limit of normal PSA levels for a guy my age is 2.5 ng/mL. So, though my urinary and sexual functions were back to normal, I had a mildly elevated PSA.
As mentioned at the beginning of this post, I had a repeat PSA test on June 3, 2020 – the PSA level was 1.75 ng/mL, i.e., well within the age-adjusted normal range.
Steps I Took to Lower My PSA Level
Between the two PSA tests (a period of 48 days), I was determined to see the PSA level come down, mainly because it had a large bearing on whether I could safely continue road cycling. I took the following steps:
- Abstinence from cycling. Other than a 10-minute ride to my local bike shop (LBS) on May 20, 2020, to upgrade the pedals on my bike, I had not cycled, even when the country eased its lockdown restrictions in the Conditional Movement Control Order, effective from May 4, 2020. On May 20, 2020, when I did cycle to my LBS, I wore a pair of padded bike shorts under my G&F commuter shorts to protect my boy parts.
- Avoidance of ejaculation for three weeks. My urologist told me ejaculation increases the PSA level. A three-week period of sexual abstinence was highly conservative. Based on the material available on the Internet, ejaculation may raise the PSA level for up to 48 hours. Still, I wouldn’t argue with my urologist, given his experience and expertise.
- Not straining when urinating. If there was an obstruction in my urinary tract distal the prostate, straining might excessively raise the intra-prostatic urethral pressure.
- α-Adrenoreceptor antagonism. α-Blocker medications help lower the intra-prostatic urethral pressure. I continue to take terazosin 1 mg once a day at bedtime and will do so until my next urology appointment in four months.
- Abstinence from vigorous exercise for 32 hours before the PSA test. My last workout before the test was a 10.30 km night run.
- A tomato a day. I added one tomato, eaten raw, per day to my diet, hoping the lycopene in the tomatoes would lower my PSA level.
- Occasional soybean pudding. To add some soy to my diet, I have been eating soybean pudding, a popular local dessert, once a week.
My Take on What Happened Down Below and Wrap-Up
Summing up, this is what I believe happened:
- I lowered my bike stem by 17 millimeters but did not check/adjust the saddle angle.
- Instead of a slight downward, forward tilt, I mistakenly adjusted the saddle to a neutral position, which heightened the risk of the saddle exerting more pressure on my perineum, either while riding or when I was dismounting. After one ~32km ride, I adjusted the saddle to give it a 2° downward, forward tilt.
- On two trips to my LBS in mid-March 2020, I did not wear padded shorts. Though these trips were short, the total time my perineum did not have any padded protection while I was on my bike was about 53 minutes.
- I also had poor technique dismounting from my bike – the nose of my saddle often hit my perineum.
- The pressure effect on the perineum – from the lack of downward, forward tile of the saddle, insufficient padding of the perineum while cycling, and poor dismounting technique – caused injury to the right and left pudendal nerves or one or more of their branches. The mechanism of injury was by compression of those nerves (or direct trauma to them) or by restricting their blood supply (via the pressure effect in the perineum).
- The pressure effect also temporarily restricted or occluded penile perfusion, a significant contributor to my erectile dysfunction.
- Through ischemia or compression, the pressure effect on the perineum injured the deep branch of the perineal nerve, which is a branch of the pudendal nerve. The deep branch of the perineal nerve supplies the sphincter urethrae muscle (male external sphincter muscle of the urethra), which sits inferior to the prostate in the deep perineal pouch. The resultant malfunctioning of this muscle affected urination (micturition), in that the muscle could not relax when I attempted to pass urine.
- An alternative scenario was a spasmodic urethral stricture, i.e., spasmodic contraction of the muscle fibers around the urethra, possibly from injury to the nerve supply or traumatic injury to the urethra (from the saddle pressing against the perineum).
- The obstruction of urinary flow in the urinary tract because of abnormal contraction of the sphincter urethrae muscle or spasmodic urethral stricture created back pressure as I strained to push the urine through the obstruction. The pressure might have injured the prostate, hence elevating my PSA level.
- The pain in the perineum and glans penis during and after urination was probably referred from the prostate.
- A period of abstinence from cycling allowed recovery of the damaged nerves and blood supply on or around the perineum, thereby facilitating the return of normal urinary and erectile function.
- The normalization of my PSA level was mainly because of the restoration of normal urine flow through the prostatic urethra.
With the PSA test on June 3, 2020, showing a normal level, I got the all-clear from my urologist to resume cycling (without me even asking!).
![]()
![]()
![]()
![]()
![]()
Thank you so much
Keep your writing habit up
Hi! Thanks for that informative article! It helped make me realize that maybe my health problems are caused by cycling (more precisely by a bad saddle and low-quality padded bike shorts).
Like you I have urinary hesitancy, in a much milder form though. I also similar problems with bowel movements. It started gradually over a year ago, but I didn’t think much of it because it’s not problematic enough to warrant an expensive visit to the doctor.
I now think thanks in part to your article that it probably is a medical issue (and may get much worse), so I’ll consult a doctor in the near future.
Though I really hope I don’t need to abandon cycling forever!
Hi Amerillo,
Thank you so much for your comment.
It does sound like your urinary and bowel symptoms could benefit from a visit to your general practitioner. I hope your symptoms improve soon.
You make a good point about balancing medical necessity and monetary cost – I too do this all the time. At the onset of symptoms, I just hope they will go away without any intervention. If/when they don’t disappear spontaneously, I consider different factors, including:
Speaking for myself, the wait-and-see, aka “do-nothing,” approach works only for acute conditions, e.g. a cold or musculoskeletal pain from vigorous or unaccustomed exercise. If/When my symptoms are recurrent or persistent (eventually found to be due to ulcerative colitis, irritable bowel syndrome, spinal nerve root impingement, carpal tunnel syndrome, pudendal neuralgia, to name a few), and especially when they get disabling and annoying, I invariably seek professional medical attention. For me, the two strongest motivators for getting expert opinion are:
Hi. Very informative article. I am 70 and now cycle about 100 hilly miles a week. I recognise and have experienced all the symptoms. (Also suffered from UC and colectomy in my twenties.)
At the moment my doc has remotely (due to Covid) diagnosed severe prostatitis and I am on my second course of antibiotics, which do not seem to be working. Got my prostate scoped last year and PSA is good, but consultant suspects and old urethral trauma may be causing a stricture. (At the moment avoiding a TURP)
Incidentally, my condition seems to be greatly improved after a long hard ride and lasts for the next day. (I always have a rest day off) however symptoms come back with a vengeance when I am sedentary.
My personal theory is that the vigorous cycling coupled with a high liquid intake ‘flushes’ the pipes and helps the endorphins. More so in the summer, when it is warm (higher fluid intake and longer rides?). I often experience, what I can only describe as a flushing sensation, during a ride. Thereafter all discomfort subsides. Also, I used to experience incidents of peeing Uric, crystals but that has disappeared since I upped my cycling mileage in retirement with a group of ‘Pedalling Pensioners’. (We all seem to have prostate problems!!!)
Hope you keep up the cycling.
PS It’s maybe all that coffee, cake and post ride alcohol that’s the problem with us cyclists!
Hi James,
Thank you for sharing your experience! I feel so encouraged reading that you continue to enjoy cycling despite your medical woes. It’s interesting you find cycling helps your water works, though I don’t understand how that happens. I haven’t felt any “flushing sensation” but it sounds delightful! 😃 I tend to think cycling not only provides physical health benefits, but also an avenue for social interaction (with the obligatory refreshments we cyclists take on our group rides) – much needed, especially in these COVID-19 times. Left-sided sciatica has prevented me from cycling these last few weeks – I look forward to returning to the saddle once it settles down.
I hope you recover from your acute prostatitis soon.
Hi, thanks for sharing! Im experiencing some of your symptoms right now the urinary hesistancy and specially ED. Been cycling for a year and I sometimes have a numb genitals during long ride it started when I changed to aggressive road bike last nov 2021, I search online and found out that it was my perineum that was on pressure in the saddle, I sometimes have to use sexual supplement as I cant maintain or get an erection. I had a 2 weeks rest now from cycling and just bought last week a selle smp well M1 saddle.
Sorry for my english 😂
Hi Cycling enthusiast,
It does sound like we’ve experienced similar symptoms from a more aggressive riding position. Fortunately, my ED resolved without me having to resort to any medication.
I hope your new saddle works out well for you and you will be able to start cycling again soon. In my case, it took a few small adjustments to get the optimum saddle tilt for pressure release and comfort. I haven’t tried an SMP Selle Well M1 but the Selle SMP Dynamic has been amazing for me.
Incidentally, I’ve been eyeing the SQlab 612 ERGOWAVE® active 2.1 saddle lately because it promises relief of pressure on both the perineal area and intervertebral discs. You see, in addition to my history of bicycle seat neuropathy, I also suffer from left-sided sciatica. In fact, I’m currently going through an acute episode. Therefore, I’m staying off the saddle for now, but when I resume cycling, I suspect/hope a reduction of pressure on my intervertebral discs will lower the risk of aggravating my sciatica.
By the way, your English is perfectly fine!😃
Dear Dr Teh
I found your article very interesting, informative and helpful. I was struggling to know how to proceed as a result of my symptoms but I am convinced that I am experiencing the same problems that you did and I feel that you have probably provided a solution.
During the pandemic for the last 2 years I have been cycling as a means of keeping fit, particularly as I have a knee problem. Prior to that, I simply kept as active as I could. During this last winter I only cycled infrequently, mainly because of weather ( rain and head winds ).
Just over 2 weeks ago,the weather became suitable and stable so I restarted cycling every day. At my age (84), I only go for 10 – 15 km at a modest speed. My knee has benefitted but I developed urinary problems, increased urgency and frequency, a very slow stream, slow to stop and sensations of itching/burning in the urethra towards the tip of the penis. The urgency, hesitancy and frequency problems were more acute at night, necessitating visiting the toilet every 30 mins to 1 hour, with shallow sleep in between.
I consulted the GP, who prescribed an antibiotic, although the urine sample didn’t show evidence of infection on the “litmus” test. It was more of a “try it and see if it works” situation. It didn’t, so he prescribed tamsulosin for improving the stream and suggested having a check on whether the bladder was emptying completely.
At this point, I read your article and concluded that I was probably suffering from the bicycle saddle causing urethral irritation/injury. It’s not clear why this hasn’t happened before but it seems to coincide with returning to cycling after a 3 – 4 months winter break. I (and the GP) discounted prostate as I had brachytherapy some time ago and my PSA has been steady at less than 0.01 ng/mL.
However, I should like to ask you if the prostate can expand for other reasons to produce some of the symptoms, while the PSA remains so low? Also, is there any virtue in my asking for terazonin?
I am now stopping cycling for a while to see if the symptoms subside, before revisiting the GP ( expensive where I live ). If so, I shall change the saddle for one of those mentioned in your article and also get padded shorts. Hopefully, I can restart cycling daily.
Hello Frank,
I’m sorry to hear about your urinary symptoms.
Based on your information, I believe you have two risk factors for developing the symptoms you mentioned, i.e., advancing age and prostate brachytherapy. Everyone’s waterworks deteriorate with age, and brachytherapy can cause tissue scarring and stricture of the urethra.
However, symptoms arising from age or radiation damage worsen over an extended period. Your symptoms developed quickly, which makes me suspect the two weeks of cycling precipitated them.
Taking a break from cycling until your symptoms improve was prudent.
Can the prostate enlarge despite a low PSA level? In theory, brachytherapy spares healthy tissue. Therefore, the remaining prostate tissue after treatment might grow. However, because your PSA is so low, it seems unlikely that any growth of prostatic tissue is the problem underlying your urinary symptoms.
Should you try terazosin instead of tamsulosin? Terazosin and tamsulosin belong to a class of drugs called alpha-blockers. Both medicines relax the smooth muscle in the prostate and urethra, which helps you pass urine more easily. Terazosin and tamsulosin are comparable in improving urinary symptoms and flow. One potential problem with alpha-blockers is orthostatic hypotension, also called postural hypotension. Using terazosin, a non-selective alpha-blocker, carries a higher risk of orthostatic hypotension than tamsulosin, a selective alpha-blocker. I believe tamsulosin is a reasonable choice of alpha-blocker in your case.
Reducing the pressure on your perineum by trying a different saddle and wearing padded shorts when you return to cycling sounds like an excellent idea.
I hope your symptoms improve and you can get back on your bike soon.
Thank you very much for your candid and detailed article. Please keep us posted on your situation and your choice of saddle.
I have ED and urinary frequency issues and am seeing a urologist this month.
I really don’t wish to give up my cycling but if i means that or the symptoms I suppose I have no choice. I have bought a wider, fatter saddle which allows me to sit back on my buttocks more on my mountain bike (used mainly on roads) and hopefully this should help.
Hello Szuhel,
Fortunately, my genitourinary symptoms have not recurred since April of 2020. Everything seems to be working fine down there. In addition, annual PSA checks have produced normal results.
As for my saddle, I’m still using a Selle SMP Dynamic. It has served me well over the past couple of years. Nevertheless, the SQlab 612 ERGOWAVE® active 2.1 saddle continues to pique my interest. I might buy one later in the year; if I do, I’ll be sure to post a review on this blog.
I hope your new saddle helps and your symptoms resolve before long.
Thank you for your detailed article.
I think I’m struggling with the same issue as I switched to a road bike about a month ago and started cycling daily.
My symptoms perfectly match yours, even though I’m 25, and the onset was gradual but at some point started getting out of hand. I decided to take a break from cycling yesterday and scheduled a urologist appointment.
I was wondering though, how long did it take you to notice an improvement after quitting cycling?
Hi John,
I’m sorry to hear about your health woes.
My symptoms probably developed gradually too, but I noticed them only when they got severe after about four weeks.
For that episode in early 2020, I stopped cycling on March 17. My urinary symptoms started improving on March 26, i.e., nine days later. The 9-day break from cycling and the addition of terazosin (Hytrin) on March 26, which my urologist prescribed, could have contributed to this improvement.
My urination improved further over the next couple of weeks, and I was back to normal by April 7, 2020. So, it took about three weeks from the time I stopped cycling to the complete resolution of urinary symptoms. My erectile dysfunction took about the same time to recover.